March 15, 2018 (1:14 pm) — The three manufacturers of duodenoscopes sold in the U.S. have not complied with the requirements of an order the FDA issued to each in 2015, according to individualized warning letters the FDA sent each company last week.
 More than two years ago, on October 5, 2015, the FDA ordered these manufacturers to perform two types of studies — called postmarket surveillance studies — to understand, in part, factors that might contribute to a reprocessed duodenoscope remaining contaminated with multidrug-resistant bacteria.
More than two years ago, on October 5, 2015, the FDA ordered these manufacturers to perform two types of studies — called postmarket surveillance studies — to understand, in part, factors that might contribute to a reprocessed duodenoscope remaining contaminated with multidrug-resistant bacteria.
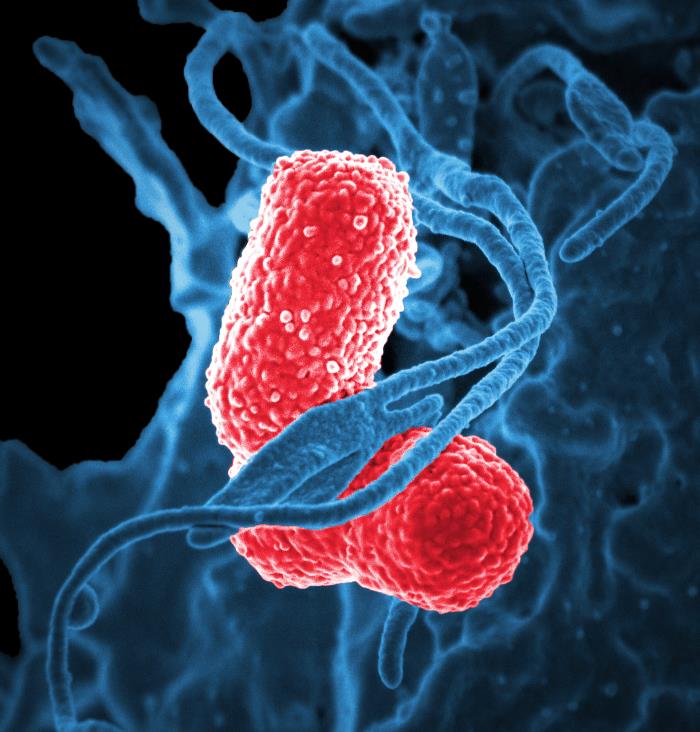
Outbreaks of multidrug-resistant bacteria linked to duodenoscopes have been reported in the U.S. and Europe despite apparent confirmation that endoscopy staff were correctly cleaning and disinfecting the device in accordance with the manufacturer’s reprocessing instructions, the FDA and a January 2016 U.S. congressional report have concluded.
The three warning letters the FDA issued last week, one to each manufacturer dated March 9, 2018, may be read here: (1) Fujifilm Medical Systems USA, Inc., (2) Olympus Medical Systems Corporation, and (3) Pentax of America.
The FDA’s order — called a 522 Order — requiring each duodenoscope company perform these surveillance studies follows on the heels of a public notice the FDA had issued eight months earlier that same year.
In that public notice released on February 20, 2015, the FDA advised that the complex designs of duodenoscopes — which feature a forceps elevator mechanism — may impede effective cleaning and high-level disinfection. The FDA added in this safety alert that duodenoscopes can therefore pose a risk of transmitting multidrug-resistant bacteria, including “superbugs” called CRE, to patients undergoing ERCP.
The first of the two studies the manufacturers were ordered to perform, called a “Sampling and Culturing Study,” requires each “to sample and culture reprocessed duodenoscopes that are in clinical use to learn more about issues that contribute to contamination” of the manufacturer’s models.
Last month, the FDA, Centers for Disease Control and Prevention (CDC), and the American Society for Microbiology (ASM) released voluntary, updated standardized protocols for duodenoscope surveillance sampling and culturing.
The FDA’s second mandated study, called a “Human Factors Study,” requires the three manufacturers, additionally, to evaluate hospital staff’s compliance with the duodenoscope manufacturer’s reprocessing instructions.
Manufacturers of reusable devices, including duodenoscopes, are required to validate the device’s reprocessing instructions, not only for effectiveness, but also to ensure that users can successfully understand and execute these instructions.
The FDA’s 522 Order issued to each duodenoscope manufacturer in October 2015 is so named because section 522 of the federal Food, Drug, and Cosmetic Act — or, “the Act” — grants the FDA the authority to require manufacturers of duodenoscopes (and certain other class II or class III medical devices) to conduct these specific postmarket surveillance studies, as required.
Duodenoscopes, ERCP
Duodenoscopes are a type of GI endoscope used to perform endoscopic retrograde cholangiopancreatography (ERCP). Diseases of the liver, bile ducts, and pancreas may be diagnosed and treated during ERCP, which is performed more than 500,000 times a year in the U.S.
An adjustable forceps elevator mechanism is located at the duodenoscope’s distal tip. A thin wire that is enclosed in a narrow, dedicated channel (that is often sealed) connects this cantilevered mechanism to a manually-controlled knob on the endoscope’s control body. This knob is used to angulate this mechanism and, in turn, direct and introduce an accessory, such as a guide wire or cannula, into the common bile duct during ERCP.
Advising that the complex designs of duodenoscopes can impede effective reprocessing, the FDA further instructed in its February 2015 safety alert that “meticulously cleaning duodenoscopes prior to high-level disinfection should reduce the risk of transmitting infection, but may not entirely eliminate it.”
Three questions
More specifically, the FDA ordered these postmarket surveillance studies be performed to address the following three questions, which the FDA’s warning letters ask of each manufacturer, about the cleaning and disinfection of duodenoscopes in real-world settings, such as a busy endoscopy unit:
1. “Are the user materials that are included in your firm’s duodenoscope labeling and instructions for use sufficient to ensure user adherence to your firm’s reprocessing instructions? (Note: User materials include user manuals, brochures, and quick reference guides from the manufacturer that are provided to the reprocessing staff) (Human Factor Study)”

2. “After use of your firm’s labeled reprocessing instructions, what percentage of clinically used duodenoscopes remain contaminated with viable microorganisms? (Sampling and Culturing Study)”
3. “For devices that remain contaminated after use of your firm’s labeled reprocessing instructions, what factors contribute to microbial contamination and what steps are necessary to adequately decontaminate the device? (Sampling and Culturing Study)”
According to the FDA’s warning letters issued last week, these three manufacturers have failed “to provide sufficient data to address the postmarket surveillance studies requirements under Section 522 of (the Act).”
“The FDA takes these violations very seriously and will continue to monitor these manufacturers to ensure they take appropriate corrective action and this important public health information is obtained,” the agency wrote in a webpage it has developed — “Infections Associated with Reprocessed Duodenoscopes” — that provides the public with important information about these ordered surveillance studies, along with other updates about duodenoscopes.
The requirements of the FDA’s October 2015 orders notwithstanding, these warning letters state that, to date, one manufacturer has not begun to collect the surveillance data from reprocessed duodenoscopes, and the other two have not provided the FDA with sufficient surveillance data. Only one of the three manufacturers has complied with the requirements of its respective human factors study, the FDA’s press release states.
Quality, Safety and Case Reviews: Click here to read about Dr. Muscarella’s quality and safety services designed to help clients reduce the risk of healthcare-associated infections, including superbug outbreaks linked to contaminated duodenoscopes and other types of reusable medical equipment.
Seven identified duodenoscope models
Last week’s three warning letters state that each company “has committed a prohibited act under section 301(q)(1)(C) of the Act by failing to comply with requirements under section 522 of the Act.” The FDA’s letters note further that the following seven (7) duodenoscopes models are “currently misbranded” [under section 502(t)(3) of the Act]:
- Olympus JF-140F, PJF-160, TJF-160F, TJF-160VF, and TJF-Q180V models
- Pentax ED-3490TK model
- FujiFilm ED-530XT model
Previously, the FDA had issued these manufacturers several “decision letters” since February 2017 (and, again, in January or February of this year) advising that the company was “not meeting the milestones per the agreed study plan and timeline,” the three warning letters disclose.
CRE, carbapenem antibiotics and colistin

(Source: FDA)
The FDA noted in last week’s three warning letters that it ordered these postmarket surveillance studies be performed “because failure of (duodenoscopes) would be reasonably likely to cause infection and possibly death in patients undergoing (ERCP) …”
CRE, or carbapenem-resistant Enterobacteriaceae, are “nightmarish bacteria” resistant to powerful carbapenem antibiotics, but often can be treated by another antibiotic called colistin.
In August, a case linking a duodenoscope (the ED-3490TK model) to probable transmission of a superbug resistant to colistin — the “last resort” antibiotic — was documented in the FDA’s medical device database. Colistin-resistant bacteria pose a significant and emerging threat to public health in the U.S. and globally.
This case of probable transmission — discussed for the first time in the related article, “A Duodenoscope Has Been Linked to ‘Probable Transmission’ of a Colistin-Resistant Superbug” (December 8, 2017) — may document the first instance that an infection caused by a colistin-resistant superbug was linked to a duodenoscope and ERCP.
Three bacterial clusters reported in 2017
Last year a manufacturer filed three regulatory reports with the FDA linking another duodenoscope (the TJF-Q180V model) to three unrelated clusters, or outbreaks. These infections appear to have occurred in Europe, possibly in France, and were reported separately to the FDA in February, August and November (of 2017).
One of these three regulatory reports is discussed in a related article, “The Redesigned Olympus Duodenoscope Has Been Linked to a ‘Superbug’ Cluster” (March 21, 2017). The other two reports appear not to have been previously disclosed or discussed until now.
Two of these three regulatory reports identify oxa-48-producing Kl. pneumoniae, which are CRE, as the cause of the infections. Pseudomonas aeruginosa is the bacterial strain cited in the third report’s case, which was discussed in more detail last year in the Los Angeles Times (March 22, 2017).
The majority of disclosed “superbug” outbreaks linked to ERCP performed in the U.S. and Europe occurred between 2012 and 2015. Few cases identified in 2017 have been publicly discussed.
Technical Consultant: Dr. Muscarella provides expert opinions, case reviews and advice for hospitals, device manufacturers and consumers about the causes of healthcare-associated infections (“HAIs”) linked to contaminated upper and lower GI endoscopes, among other devices. Contact him (using your smart phone): Email | Text (SMS) | Skype
Article by: LFM Health Solutions, LLC. Lawrence F Muscarella, PhD., President Posted: March 15, 2018. LFM Healthcare Solutions, LLC. Copyright 2018. LFM Healthcare Solutions, LLC. All rights reserved.
Lawrence F Muscarella PhD is the owner of LFM Healthcare Solutions, LLC, a Pennsylvania-based quality improvement and consulting company that provides safety services for hospitals, manufacturers and the public. Email Dr. Muscarella for more details.
May 2015 Advisory Committee Meeting FDA
4. Supplemental Measures to Enhance Duodenoscope Reprocessing
At the Advisory Committee meeting, representatives from several health care facilities and the panel discussed additional strategies that they have implemented to reduce the risk of infection transmission, such as: microbiological culturing, sterilization, use of a liquid chemical sterilant processing system and repeat high-level disinfection. In each case, staff applied these supplemental methods in addition to meticulous cleaning as part of strict adherence to the manufacturer’s reprocessing instructions.